Often called the "quintessential" minimally invasive heart surgery, minimally invasive direct coronary artery bypass, or MIDCAB, follows the basic premise of conventional coronary artery bypass graft surgery (CABG), but in a truly minimally invasive fashion. Whereas CABG requires cardioplegia to stop the heart, the use the heart lung machine for cardiopulmonary bypass, and a 30 cm. long, sternum-splitting incision, MIDCAB doesn't utilize the heart lung machine or cardioplegia and only uses a tiny incision that avoids splitting the sternum bone. Through this small 10-12 cm access incision in the patient's chest, the surgeon connects a graft to diseased coronary arteries on a beating heart without any artificial support to the circulation. Due to the nature of the operation, suturing must be done under direct vision and the coronary artery to be bypassed must lie directly beneath the incision. Consequently, this procedure is only designed to bypass one or two coronary arteries. Ultimately, however, this procedure provides the most minimally invasive heart surgery alternative to limited CABG and angioplasty that is practiced today.
Procedure
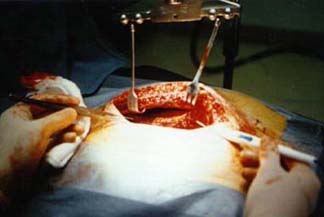
Once the patient is anesthetized, the surgeon makes a 10
cm. long transverse incision on the front of the chest, towards
the left side. This incision is then deepened to divide the pectoral
muscles. When the rib cage is reached, a small portion of the
front of the rib is removed [1]. The picture in the center shows
the MIDCAB incision compared to a conventional CABG incision (denoted
by the X's).
Once the chest has been opened and retracted, an internal mammary
artery, IMA is harvested. The IMA originates from the subclavian
arteries (that run beneath the shoulders and provide blood to
the arms) and then run parallel down each side of the front of
the chest and connect with small arteries under each rib. The
IMA may be taken for use in coronary artery bypass grafting and
minimally invasive direct coronary artery bypass procedures since
the small arteries beneath the ribs provide a secondary source
of blood for the area.
After the IMA is harvested, the frame for the MIDCAB instrumentation
is fitted onto the incision. Several instruments must work in
conjunction to make operating on a beating heart feasible - these
will be discussed in detail later in techniques and technology.
For this procedure, the heart stabilizer limits the movement of
the heart to within 1 millimeter of motion, thereby permitting
the surgeon to operate. A site blower removes blood from the field
of operation, providing a clear view and a site light gives illumination
while a site manipulator moves the heart.
Once the IMA has been collected and the MIDCAB instrumentation
is in place, the surgeon commences the bypass in much the same
way as a conventional CABG. The surgeon makes an incision in the
pericardium thereby exposing the left anterior descending coronary
artery (LAD). One end of the IMA is attached to the artery of
the beating heart - before the blockage - with sutures, and the
other end is sutured to the LAD after the blockage [2]. The IMA
therefore serves to divert blood around the clogged section of
coronary artery. Once the IMA is in place, the MIDCAB instrumentation
is removed and the patient is sewn up.

This procedure is more difficult than conventional bypass for two reasons. First, the surgeon must maneuver through an incision that it approximately one third (12 cm) of the size of the incision in conventional CABG (30cm). Secondly, the surgeon is operating on a beating heart, which means both movement and blood; two issues not present in conventional CABG. Therefore, this procedure requires much more skill and manual dexterity than conventional CABG [2].
MIDCAB vs. CABG:
Conventional CABG has been around for the past four decades, and in that time it has nearly been perfected. Although more than 1 million of these procedures take place annually with a 99% success rate, this is still a very traumatic and painful surgery for the patient.
Conventional CABG is performed through a 30 cm. vertical incision which splits the patient's sternum bone. During CABG, the heartbeat is stopped temporarily by either cardioplegic arrest or fibrillatory arrest and the blood circulation is maintained artificially by a heart-lung machine [1]. Once the heartbeat is stopped, the surgical connection between the graft and coronary artery can be achieved with greater ease and precision than if the heart were to continue moving.
Conventional CABG is the gold standard in heart surgery for two main reasons. First, working on a non-beating heart allows for more efficient and more precise anastomosis. Second, and more importantly, CABG has been tried and tested making it widely accepted as the best heart surgery. As will all medical technologies, surgeons are reluctant to haphazardly switch from a procedure or a device with years of high success and proven reliability to a recently developed procedure or device which may look better intuitively and on paper but has not shown the same reliability and success.
However, CABG is not without complications and disadvantages:
* Patients are in surgery and under anesthesia for around 6
hours consequently increasing post-operative intensive care treatment
* The 30 cm., sternum-splitting incision is cosmetically displeasing
and increases pain, discomfort, and hospitalization time for the
patient.
* Patients often require blood transfusions
* Long surgery and hospital stays lead to high costs (~ $35,000/CABG).
* CABG often requires months for full recovery
In addition, cardiopulmonary bypass (the heart lung machine) is associated with a number of serious complications [9]:
* Fluid shifts in the body and depression of the patient's
immune system.
* Postoperative bleeding from inactivation of the blood clotting
system as it passes over the artificial surfaces in the heart-lung
machine.
* Hypotension associated with heart-lung machine may cause renal
failure and ischemia of the brain.
* Recently, a number of strokes and neurological deficits, as
many as 25,000 a year, have been linked to the use of the heart-lung
machine.
* Further problems with the Heart-Lung Machine
Several recent studies propose significant benefits of MIDCAB over CABG:
* The procedure is performed in only two to three hours, compared
to three to six hours for a traditional bypass.
* The recovery time is dramatically reduced from months, to days
or week.
* Complications associated with the heart-lung machine are avoided.
* There is a reduced need for blood transfusions, if any.
* Due to less time under anesthesia, patients are moved out of
intensive care more quickly.
* Patients tend to experience less pain and discomfort than CABG
patients.
* The 10 cm. incision is cosmetically more acceptable than a 30
cm one.
* Initial figures estimate up to 40% savings off the cost of conventional
CABG.
* A recent study showed a significantly higher quality of life
for MIDCAB patients compared to CABG patients [9].
* According to several studies, MIDCAB has shown a 90% effectiveness
rate in worldwide studies and has provided substantial relief
to approximately 95% of all patients undergoing the procedure.
Disadvantages of MIDCAB:
While MIDCAB is easier on the patient and is probably less expensive than traditional CABG, the disadvantages of MIDCAB compared with traditional CABG are substantial. First and foremost, MIDCAB is only a plausible alternative to CABG surgery involving one or two arteries, not all CABG surgeries. Secondly, minimally invasive surgeries, including MIDCAB, only comprise around 10% of total heart surgeries, so exposure is limited [11]. Additionally, allowing the heart to continue beating during MIDCAB makes the performance of the anastomosis more difficult and significant ischemia during the procedure may lead to hemodynamic compromise of the patient, so cardiopulmonary bypass must be available [11]. In a few cases, urgent conversion to conventional open-chest methods has also been necessary. Finally, MIDCAB has only been around for the past 5 years, so long term results of the procedure have yet to be determined, but current estimates look promising [12].
William R. Mayfield, M.D., an Atlanta-area surgeon developing advanced endoscopic techniques for heart surgery says the fact that preliminary results with the new techniques have not equaled those of the old standards should not be cause for concern. ''That just tells me we're working with first-generation instrumentation, a lack of training and a lack of standardization,'' he says. ''I'm very confident we'll soon be able to match open-heart surgery" [16].
MIDCAB vs. Angioplasty:
Given the fact that MIDCAB can only be used for patients with one or two damaged coronary artery, perhaps a comparison to angioplasty is a better gage of MIDCAB's worth and potential. During angioplasty, a x-ray guided balloon catheter, comprised of a long flexible tube with a small inflatable balloon on the tip, is inserted into the femoral artery and threaded through the aorta and into the coronary artery. Once the occluded area is reached, the interventional cardiologist inflates the balloon thereby compressing the plaque and increasing the diameter of the blood vessel [10]. Often times, a stent, a small metal retainer used to physically restrain plaque, is placed around the balloon then employed in the occluded artery when the balloon inflates. Around 700,000 angioplasties take place each year at a cost of around $20,000 per procedure [10].
Angioplasty has become a popular alternative to single CABG for a few main reasons. First, angioplasty is far less invasive than CABG - no chest wound or scaring. Additionally, angioplasty is both less expensive ($20,000 compared with ~ $35,000) and less painful than full-blown CABG. Finally, Angioplasty patients also require less recovery time and can return to work faster.
However, angioplasty also a few major drawbacks. First and foremost, reports have shown that around 50% of angioplasty procedures require revascularization within five years due to restinosis. In addition, the same reports show that more angioplasty patients suffer from angina after five years [10].
MIDCAB has been proposed as the best alternative to angioplasty because, at least in current studies, MIDCAB seems to produce more definitive results for patients with single vessel disease for around the same amount of money. Whereas an angioplasty procedure may need to be redone within five years, MIDCAB procedures show similar long-term success with conventional CABG. The drawbacks are that MIDCAB is still more invasive than angioplasty and general anesthesia is necessary, and MIDCAB hasn't been around long enough to know long-term effects and success [11].
Therefore, at least for now, the role of MIDCAB in patients with single vessel coronary disease will be limited to those who require interventional therapy but are not suitable candidates for angioplasty [11]. This includes patients who have either undergone one or more failed angioplasties or have elected for surgical revascularization instead. Perhaps if long term results conclusively prove MIDCAB to be a superior procedure, or if MIDCAB can be made so noninvasive that to be considered equally as invasive as angioplasty, then MIDCAB would become the chosen procedure for single vessel coronary disease [11].
Costs
There are no real definitive costs to MIDCAB available, however several factors make MIDCAB a more cost efficient procedure than conventional CABG. First and foremost, surgery without assistance from a heart-lung machine halves the time spent in intensive care, while saving about $1,500 in direct operating room costs. In addition, due to the small incision and absence of the heart-lung machine, the MIDCAB procedure reduces recovery time from months to weeks or days thereby allowing patients to return to work sooner. Costs are also cut because the time required for the actual surgery is less that that of conventional CABG.
Significant MIDCAB costs lie in the instrumentation. Disposable instrumentation, such as the heart stabilizer, costs between $1,500 and $5,000, while reusable tools, such as the octopus, ranges around $10,000. Many agree, however, that the emergence of a host of established companies, including U.S. Surgical Corp., Baxter International, and Genzyme that are developing a variety of competing disposable and reusable tools, will lower prices while advancing the state of the art.
According to the Center for Health Industry Performance Studies, with the average cost of traditional bypass equaling ~ $35,000, the beating-heart method should allow hospitals to shave enough in ICU and ancillary costs over traditional approaches to make the start-up hassles and instrument costs worthwhile. Current estimates show that MIDCAB costs around 40% less than conventional heart surgery.
However, while the figures look like a no-brainer, one must remember that the price for operating through small holes is paid in limits on a surgeon's ability to maneuver and perform his work. For MIDCAB, and many complex operations, that price may remain too high to change.
Eligibility, Prevalence and Scope
MIDCAB has been hailed as the "best of both worlds" because this procedure combines the proven surgical benefits of conventional CABG (much lower risk or restinosis and repeat treatments) with a less painful and traumatic outcome similar to an angioplasty procedure. However, due to the limited size of the MIDCAB incision, only certain patients are eligible candidates for the procedure:
1. Patients who have a blockage in one or two coronary arteries
located on the front side of the heart but are considered too
high risk for conventional bypass surgery or balloon angioplasty.
2. Patients who are otherwise healthy, but have a blockage in
one to two coronary arteries located on the front side of the
heart.
Today, these candidates only comprise the 5% of coronary artery bypass graph (CABG) patients that require only one bypass graph. As discussed in MIDCAB vs. CABG and MIDCAB vs. Angioplasty, possible reasons for this small percentage are the prevalence and success of CABG and the minimal invasiveness of angioplasty. MIDCAB is simply too new to threaten either of these two procedures.
However, MIDCAB prevalence is rising. By mid-1996, at least 200 MIDCAB procedures had been performed in various universities and private hospitals throughout the United States and several hundred more in Europe and South America [5]. This year (2000), it's estimated that surgeons will do 100,000 beating-heart surgeries (MIDCAB and OPCAB) - about 20 percent of all the bypass operations done in this country.
If MIDCAB continues to show similar long-term success rates
to CABG in the coming years and proves to be an effective and
longer lasting alternative to angioplasty, this procedure could
account for as many as 35% of the revascularization cases every
year. Of this 35%, 4% will come from conventional CABG cases and
31% from angioplasty procedures.
In monetary terms, MIDCAB could stake claim to more than $20 billion worth of open-heart surgery, as well as a chunk of the booming market for angioplasty. This exorbitant amount of money has drawn the attention of the medical-technology firms mentioned earlier (Guidant, Heartport, Medtronics) and many others who are developing specialized minimally invasive surgical gear. This interest has, in turn, lured Wall Street investors into this lucrative market.
For now, however, MIDCAB is limited to offering new hope and opportunities to patients who are not eligible for traditional open-heart surgery or angioplasty. And, even after the techniques are refined, the most avid boosters concede that minimally invasive approaches are likely to claim only a fraction, perhaps in the range of one in four, of the procedures now performed by traditional means. Even the most passionate optimists say that within 10 years minimally invasive approaches might be used in half of heart surgeries.